Surgery Vs. Conservative Management of Meniscus Tear in the Knee
What are the menisci?
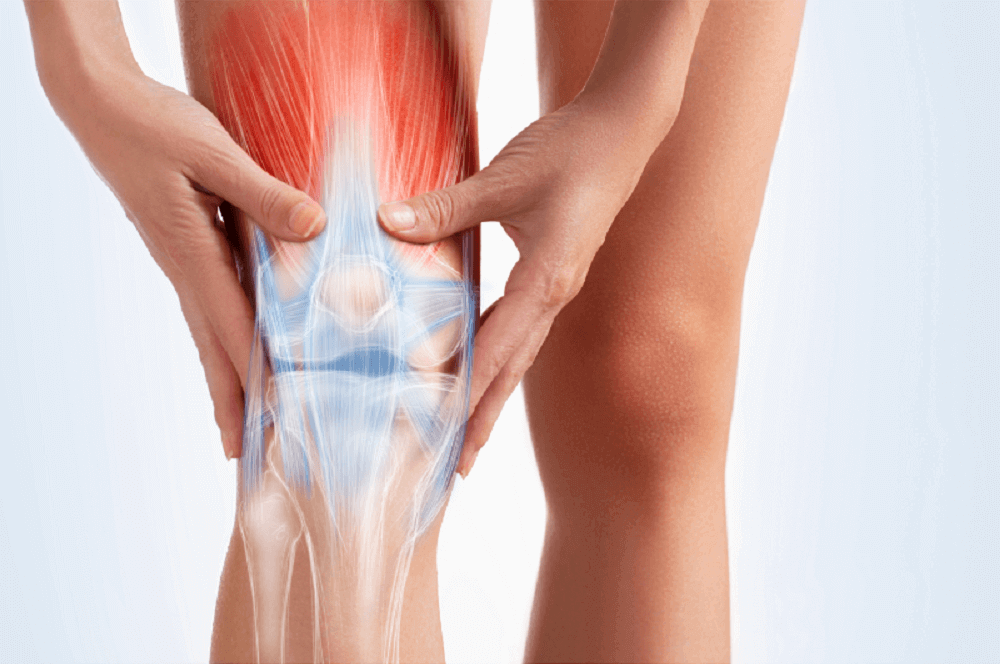
There are two menisci in each knee; the medial meniscus and the lateral meniscus. The main roles of the menisci are to help with shock absorption and distribute forces evenly across the knees, and to improve joint stability and joint contact between the femur (thigh bone) and tibia (shin bone).
What is a meniscus tear?
Tears can occur in a meniscus as a result of excessive loading, by two mechanisms. These are compressive loads (think landing from a great height), or more commonly, shear forces (common with changing direction under high speed). These can result in tearing or fraying of the meniscus edges, or in more severe cases, disruptive tears that cover a greater surface of the meniscus.
There are certain types and grading of meniscus tears, that are commonly seen on MRI scans. these are, in order of least to most severe: Horizontal tears, Parrot-beak tears, Bucket-handle tears, and complex tears. These are graded based on the location of the tear (some tears can protrude into areas of the meniscus where there is poor blood flow) & depth of the tear (length of tear, usually measured in millimetres).
Tears may not necessarily occur as a result of trauma or injury – sometimes the meniscus can be impacted in a knee with osteoarthritis (what we classify as a degenerative meniscus tear).
What are the symptoms?
At the time of injury, you may feel a click or popping sensation in the knee, followed by an onset of pain. Following this, there will be swelling of the knee joint, along with pain. Pain can be moderate to severe – but this doesn’t necessarily indicate how severe a meniscus tear is. There may be some pain with walking, particularly when trying to take body weight through a bent knee. Climbing and descending stairs may also be painful, as well as squatting movements.
Diagnosing Meniscus Tears
Allied Health Clinicians such as Physiotherapists, Chiropractors and Osteopaths are trained in the diagnosis of meniscus tears. There are a range of orthopaedic tests that help us determine whether a meniscus injury may be present, how severe it may be, and if further investigations (e.g. Diagnostic scans) are needed.
During this assessment, we should be able to determine if a meniscus tear is acute (as a result of injury) or degenerative, as well as if it is obstructive or non-obstructive. Obstructive tears often limit walking or athletic capacity as the torn ends of the meniscus get caught or “locked” in position, which is followed by collapsing or “giving-way” of the injured knee. Non-obstructive tears are still painful but often the person will not have any “giving-way”, locking, or knee instability present.
Indications for Surgery
The severity and impact on a person’s function are the two factors we need to consider before undergoing surgery. Generally, an obstructive meniscus tear will require further imaging to determine severity, and a surgical consult with a specialist knee surgeon may be of value. Severe parrot-beak, bucket-handle, and complex tears will often require arthroscopic surgery to help remove any “locking” of the knee and help that person return to full function.
Indications for Conservative Management
Conservative management is basically a non-surgical approach to meniscus tear rehab. This should be conducted with a qualified Allied Health professional, such as a Physio, Chiro, Osteo, or Accredited Exercise Physiologist.
There is good evidence for non-operative management of less severe, non-obstructive meniscus tears.
Conservative management should be structured as follows: Return to full knee range of motion and normal walking patterns, strengthening exercises of the knee (targeting the quads, hamstrings, calves and muscles of the hips), and a gradual return to full function, including sport specific rehab exercises if indicated.
A good knee meniscus rehab program should go for around 6 to 12 weeks, depending on pain levels, previous knee strength, and the person’s individual goals. For example, a person whose main goal is to return to walking 5km a day will have a very different program to a person who’s goal is to return to basketball.
Important things to consider!
Good quality, long-term evidence now suggests that knee surgeries can increase the likelihood of developing osteoarthritis of the knee later in life. When considering surgery, think critically about whether your knee is locking or giving way, or if you feel you will get a good result from non-operative management instead.
After knee surgery, you will need to do a rehab program anyway! If you have no locking symptoms and moderate pain, it may be worth starting a rehab program anyway and monitoring the medium-term effects. If this works for you, great! If not, then it may be a good idea to talk to your rehab clinician about surgical options.
Returning to sport – returning to sport after meniscus injury (for both surgical and non-surgical management) should be criteria-driven. That is, based on the function and strength of the knee, and not just pain symptoms.
About the author:
Will Ryan (BPhyt, APAM) is the Senior Physiotherapist and Director of MD Health Paddington. Will has a strong exercise-based approach to physiotherapy, including strength and conditioning principles into his rehab programs. Will can be contacted at (07) 3505 1494, or via email at paddington@mdhealth.com.au .
References:
- https://www.learn.physio/p/blogposts-mick-talks-chris-raynor
- https://bjsm.bmj.com/content/56/15/870
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6423358/
- https://pubmed.ncbi.nlm.nih.gov/19732643/
- https://pubmed.ncbi.nlm.nih.gov/21378495/
- https://pubmed.ncbi.nlm.nih.gov/17063840/
- https://www.physio-pedia.com/Meniscal_Repair

Hi, I’m Michael; Chiropractor, Dad, science enthusiast, active weightlifter and keen sportsman. I work with busy and active people who are struggling with pain to find relief from their symptoms so that they can return to an active lifestyle, get through their work day and their workouts without having to pop a pill so that they can feel happier and healthier in their body.